If your child is experiencing loud snoring, difficulty waking up from naps, restlessness, and more, you may want to look into sleep apnea symptoms. In this post, I outline my experience with diagnosing and treating both sleep apnea and surviving both a Tonsillectomy and an Adenoidectomy with my son to help with any concerns you may have.
*Important Note: This is not a replacement for medical advice, as I am not a medical professional. I am offering my personal experience and what worked for our family. If you have any concerns be sure to reach out to your pediatrician.
This was our second go-around with sleep apnea, as we had the same exact procedure with our older son. As with anything, it’s important to note that each person’s recovery is different. No matter how “routine” a procedure, it’s always unnerving for your child to have surgery and go under anesthesia. When I shared about the upcoming procedure on Instagram, there were quite a few questions, and many parents sharing about their experiences. Therefore, I thought it would be best for me to organize this post to help you all by grouping the most commonly asked questions as well as the tips that have worked for us in healing our son’s sleep issues.
Common Questions about Sleep Apnea in Kids
What Were the Red Flags Indicating Sleep Apnea?
To answer this question about my middle child, I am going to start by explaining my experience with my oldest, because my experience with him is what informed my concerns about my middle guy.
The reason we even reached out to our pediatrician in the first place was due to my older son exhibiting excessive snoring. Like, you could hear him from upstairs while we were downstairs watching Netflix bad. We originally brushed it off saying things like, “Oh, he must be really tired.” Or, “Maybe it’s just allergies, and he’s congested.” It didn’t really hit home until his preschool teacher reached out saying that he had extreme difficulty waking up from naps (numerous times). It turned out she had even let him sleep longer, while his peers began their work. Gah! Getting this notification was a bit jarring due to the importance my husband and I placed on sleep. As soon as my boys were born, we implemented a sleep routine. Naturally, I found it very shocking when I learned that my oldest was so exhausted after what I thought were great night sleeps (7p-7p with no *obvious wake-ups). The truth was, he was waking up, just not enough for any of us to notice.
My middle guy did not have the same level of snoring but did have EXTREMELY restless sleep. For example, he slept in very odd positions and very often complained of feeling tired. This was my first big warning as it is very odd for a child to do. In addition, he also would fall asleep within minutes of lying down. He also frequently complained of not having enough energy to do some of the same physical activities and afterschool things other kids his age were doing like baseball practice or Taekwondo. Instead, he would have to come home and relax. In an effort to help, we moved his bedtime earlier, but it never seemed to make a difference.
Note: Since my first baby, I have always followed Health Sleep Habits Health Child, and swear by their sleep program. I knew that if we were doing what we were supposed to, as far as meeting his sleep needs, something else must be going on.

What are Symptoms of Sleep Apnea in Kids?
As mentioned, please be sure to speak with your child’s pediatrician for more information. However, according to the research I have done the most common symptoms of sleep apnea in children include:
- Snoring
- Having difficulty breathing while sleeping
- Extreme restlessness during sleep
- Sleeping in strange positions
- Night Terrors, bedwetting, or sleepwalking
- Day time hyperactivity, irritability, agitated moods, or crankiness
- Problems in school
- Difficulty waking in the morning or from naps
- Difficulty staying awake or falling asleep during the day
*NOTE: It is also important to note that many children displaying these or related symptoms often get diagnosed with ADHD when in reality their issues are stemming from a sleeping disorder. Think about how you feel when you haven’t slept well. It often involves being impatient, easily frustrated, hyper, having difficulty focusing, being overly emotional, or demonstrating disruptive behavior. All of these side effects align with symptoms of ADHD and are easy to misdiagnose.

What Age Did You Notice or Become Concerned about Sleep Apnea?
When we first noticed sleep issues with my oldest son, he was four years old and still in preschool. As previously mentioned, his sleeping patterns truly became a concern for us when his teacher mentioned the difficulty he had waking up from naps as well as how tired he seemed to be throughout the day. As for our middle guy, we began to express concern at around the same age as our first (4 years old). He frequently complained of being tired, and hot having “good energy” as he put it. As a result, we had the sleep test done prior to COVID but had to delay and reschedule his surgery for obvious reasons. Otherwise, he would have most likely had the procedure done at 5 years old.
Why Did Our Son Need Surgery to Treat His Sleep Apnea?
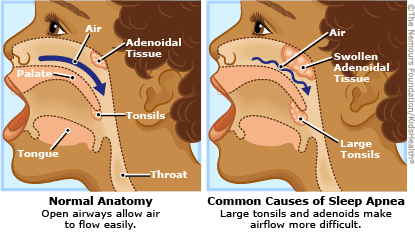
After completing a sleep study, we discovered that our son had sleep apnea. Put in simple terms, sleep apnea is a sleep disorder that is caused by some kind of obstruction or muscle relaxation of the airways during sleep. The lack of airflow can cause one’s breathing to sporadically start and stop, and it prevents sufferers from entering REM stages of sleep (this is the deep restorative sleep needed to remain healthy). After this study, the Ear Nose and Throat (ENT) doctor we consulted recommend that our son’s enlarged tonsils and adenoids
Did Our Son have Huge Tonsils Causing His Sleep Apnea?
Yes, he did have fairly large tonsils. They were first noticed by his dentist. In fact, many pediatric dentists are starting to screen for sleep concerns based on tonsils when they do their dental exams.
Tips to Identify and Treat Sleep Apnea in Kids
- Be sure that you feel comfortable with your ENT and the doctor performing the procedure. I always check a doctor’s reviews, as well as reach out to my local Facebook mom’s group to get first-hand experience.
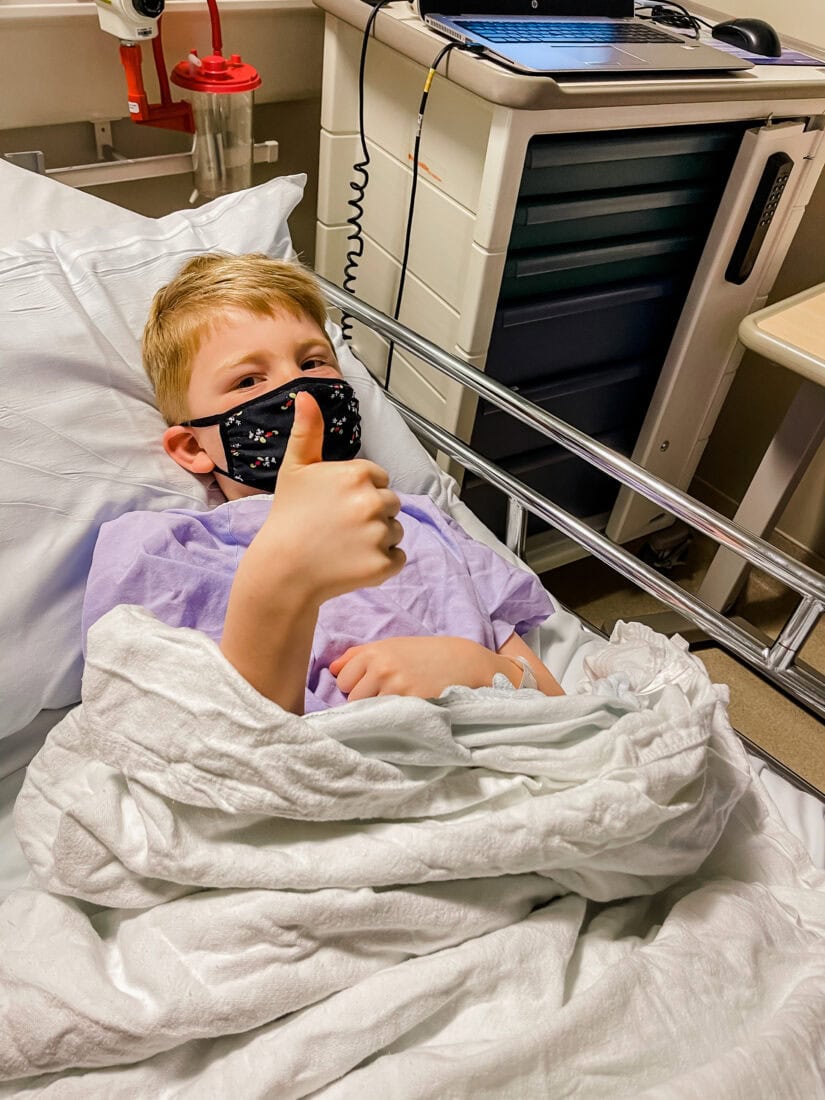
- Begin to talk with your child about what is happening, and be sure to validate those feelings of nervousness. Many hospitals will also have an option for the child to see first-hand how the process will go. With our oldest, we actually went to the hospital before the procedure, and they had photos of what my son could expect. This way he got to see what the operating room and some of the equipment would look like, making the experience less scary. They even sent us home with a book to read about what to expect and a few toys!
- Bring a comfort item to the surgery, and let your child wear their favorite pj’s. This simple trick helps to foster feelings of safety and a sense of calm.
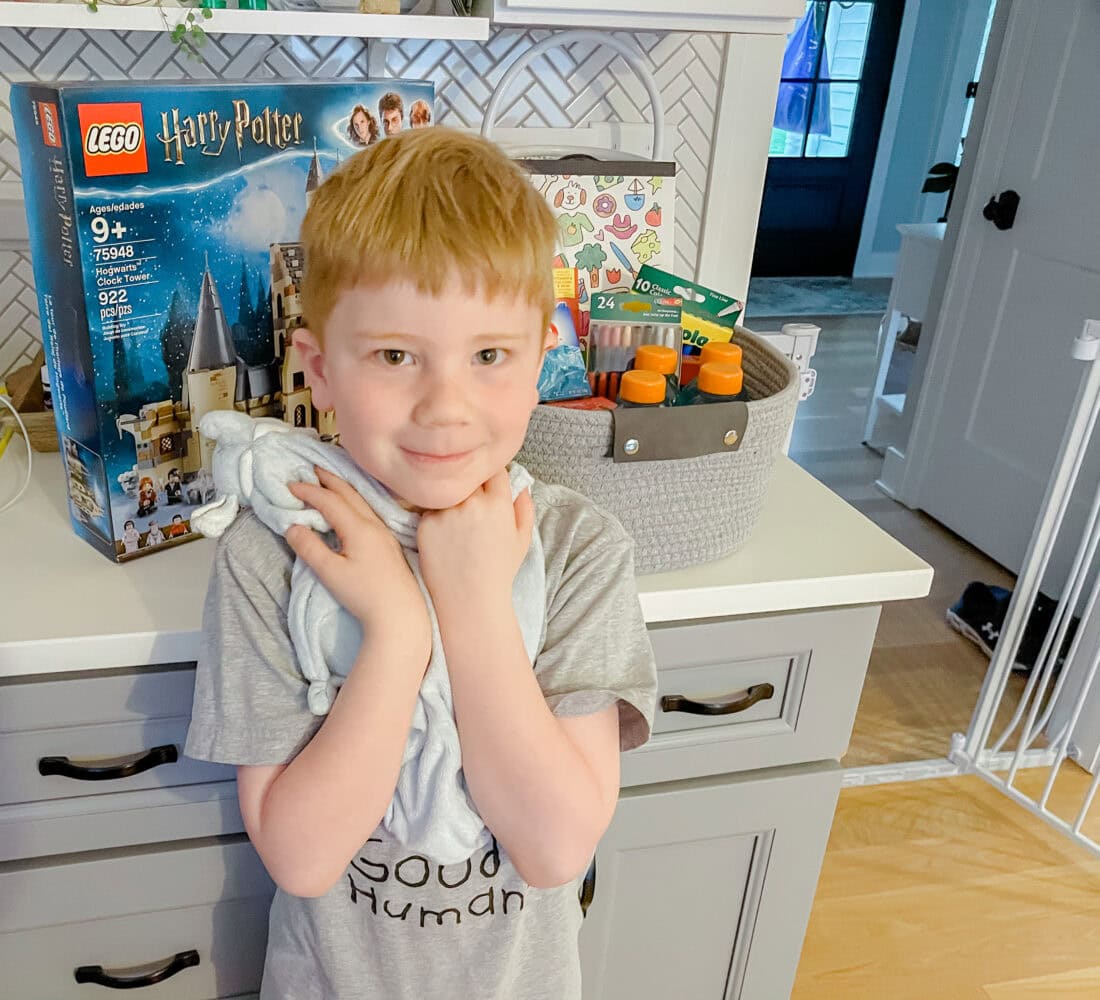
- Create something special that will happen or that they will get after the surgery. Our boys LOVE Lego and wanted a particular set. We thought it would also be a great calm activity he could do when he was tired of watching TV (yes, it happens).
- Set aside about 2 weeks for complete recovery. The actual recovery time for the surgery is suggested 7-10 days, However, I think it’s important to leave some wiggle room to allow your kids to slowly get back into their regularly scheduled program. Also, try to schedule the surgery at a time when you don’t have too many other commitments. Not only does it make the transition easier, but there is nothing quite like cuddling up with a parent when you’re not feeling your best.
- Make a little get-well basket. I kept things simple and put together a few items that might not make a normal appearance but help to ease the burden of not being able to eat all that much. These items included: Jell-O, instant soup, freeze pops, a coloring book, new crayons (is there anything better than a fresh set of crayons), a coloring pad, and a Lego set. While not necessary, I think it helps to make little one’s experiences a little more enjoyable (as enjoyable as it can be, anyway)
- Manage expectations for siblings. This step may be trickier with younger children. Yet, it’s important to know that the experience affects the family as a whole. Siblings should be aware that their brother or sister won’t be able to play as they usually do and that extra patience may be needed.
- Hydrate, hydrate, hydrate. Due to the fact that it can be challenging to swallow, it can be easy for kids to become dehydrated. To prevent this from happening, stock up on popsicles, juice, and anything else you think they might like. I found that juices with citrus, milk, and anything carbonated are a no-go as they are a little painful to swallow. However, to help monitor their intake, the doctor did mention that the goal is for your child to go potty at least once a day. If they are meeting this goal, you know they’re getting enough fluids.
- Follow the medication recommendations. We were told to alternate between Tylenol and Motrin every three hours (even during the night) for the first 24-48 hours depending on our son’s pain level. Then, we were told to switch to every 6 hours, and so on. As someone who has experienced surgery, there is nothing worse than getting behind on your pain management. So, we set our phone alarms for all the times and made notes about which medication to use and how much to give. Doing this was truly a lifesaver for those middle of the night doses! Also, when you’re putting your child to bed, remind them that you will be waking them to give them more medicine to help with the pain. I found this helpful, so as not to startle him too much.
- Use warm water to help the pain. We found that warm showers and baths were really helpful in calming our son when he began to cry due to the pain. The steam was also beneficial when he felt his throat was “too scratchy.”
- Use a humidifier at night. To help reduce mouth dryness at night, we used a humidifier to help put moisture into the air. This was really helpful because we found that our son was sleeping with his mouth open to reduce his pain.
- Diffuse oils. To create a more relaxing and calm environment, we diffused some calming essential oils. Both peace and calming and gentle baby oils were on repeat.
- Make the most out of your sofa. We made the sofa a safe haven for our son during the day. To do so, we brought all the pillows and blankets, plenty of his movies (stuffed animals), and gave him control of the remote. If there was ever a time to throw the screen time rule out the window, it’s now!
- Talk with your children. Empathize and explain that you know it is frustrating not to feel well but that the procedure is going to help with some of the symptoms you were concerned about. Be sure to give examples such as sleep loss, snoring, sleeping in their own bed, more energy, etc.
- Be patient. There is nothing fun about seeing your child in pain, and missing out on some of your own sleep. BUT, it’s really important to be patient with them and to keep talking through the process with them. Remember, this can be a scary time for your child. I promise that there is a light at the end of the tunnel, and they will feel like themselves again, probably even better!
What Other Parents Said About Their Experiences
While I shared our story on Instagram, quite a few other moms reached out and shared their experiences as well. Here’s what they said:
“… My 3-year-old girl is 9 days post tonsillectomy/adenoidectomy. She is doing great”
“Thank you for posting about this! I just asked my son’s pediatrician about this and he snores big time and definitely not overweight”
“… I am doing the same with my two-year-old at the end of the month due to sleep apnea as well. Her tonsils are practically touching apparently. …”
“My son has severe obstructive sleep apnea but his tonsils/adenoids were not enlarged so he has to wear a Cpap machine every night … It was life changing for us. The undiagnosed sleep apnea caused my son to have behavioral issues to the point the school district wanted to send him to an alternative school, but I knew something else was going on and pushed for a sleep study. He’s a completely different child now, so much calmer, happier, reasonable, thoughtful. I agree 100% that the doctors overlook this disorder and often misdiagnose as ADHD or some other behavioral condition”
“My youngest had terrible sleep apnea and turned out she had a 90% obstruction from her adenoids. She used to have the worst night terrors and snores like a trucker. Her pediatrician said it was normal but it was getting to the point where I was up with her multiple times a night. Took her to an ENT and felt terrible. I tell all the mamas now”
If you think your child is diplaying symptoms of sleep apnea, I encourage you to speak with your doctor, and if you have any further questions be sure to leave them in the comments below!
I appreciate all your love and support not only with my recipes but with your response to my son’s operation. As always, I’m overwhelmed and full of gratitude for this incredible community we have created. Please feel free to reach out via Instagram, and as always, if you share any of my recipes or creations, I’d love it if you tagged me so I can connect, see your creations, and share your page!
We’ll be back with our regular postings this week. In the meantime enjoy, and take care of yourselves, friends!
Karin
P.S. This page may contain affiliate links. Of course, you’re not obligated to use them, but I appreciate the love if you do!